As living organisms, bacteria are encoded by DNA, and DNA occasionally mutates. Sometimes genetic mutations render a bacterium immune to an antibiotic’s chemical tactics. The few cells that might escape antibiotic pressure then have a sudden advantage: with their counterparts wiped out, resources abound, and the remaining antibiotic-resistant bacteria proliferate. It’s a problem not only for the host—you or me when we are treated with an antibiotic and develop a resistant strain—but also for anyone with whom we happen to share our resistant bacteria, say, on a door handle or keyboard. In fact, most resistant bacteria develop not in people but in livestock fed antibiotics to promote growth; these resistant bacteria infect people through contaminated animal products. This is how even antibiotic “naive” people come to be infected with resistant strains of bacteria.
I see this all the time as a family doctor. A woman has a urinary tract infection. I tell her that her bacteria are resistant to this or that antibiotic, and she says, “But I’ve never taken any of those.” Welcome to the global human soup.


From the article …
Sure but they still used antibiotics and had their own production lines.
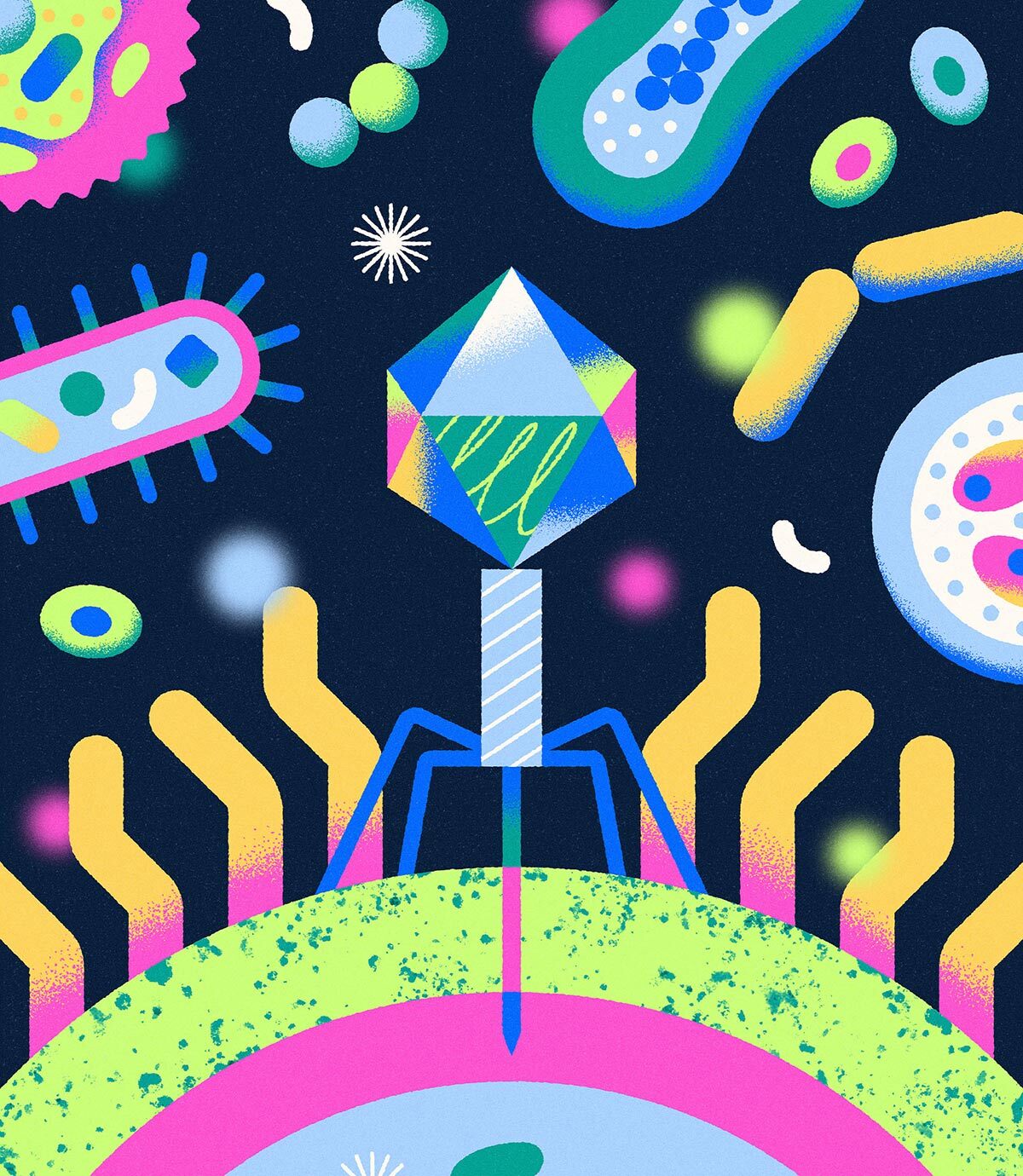
One of my professors in university was a leading researcher in bacteriophage therapy. They did some amazing things in the 2000s with them, like elimination of only pathogenic strains of E. coli in livestock. I can only imagine what they could do with a budget more inline with pharmaceutical research than that available at a small state school that most students didn’t know had a sciences department.